resources


resources


Saturday, February 28, 2009
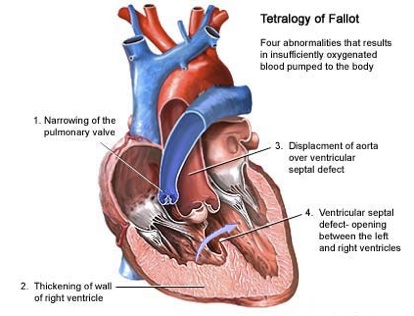
Tetralogy of Fallot refers to a group of four types of heart defects present at birth (congenital).
Causes
Tetralogy of Fallot is classified as a cyanotic heart defect because the condition causes low oxygen levels in the blood, which leads to cyanosis (a bluish-purple coloration to the skin).
The classic form of Tetralogy includes 4 defects within the heart structures:
•Ventricular Septal Defect (VSD) (hole between the right and left ventricles)
•Narrowing of the pulmonary outflow tract (tube that connects the heart with the lungs)
•An aorta (tube that carries oxygenated blood to the body) that grows from both ventricles, rather than exclusively from the left ventricle
•A thickened muscular wall of the right ventricle (right ventricular hypertrophy)
At birth, infants may not show the signs of the cyanosis, but later may develop sudden frightening episodes (called "Tet spells") of bluish skin from crying or feeding.
Tetralogy of Fallot is considered rare. Patients with tetraology of Fallot have a higher incidence of major non-heart congenital defects.
The cause of most congenital heart defects is unknown. Multiple factors seem to be involved. Prenatal factors associated with higher than normal risk for this condition include maternal rubella or other viral illnesses during pregnancy, poor prenatal nutrition, maternal alcoholism, mother over 40 years old, and diabetes.
There is a high incidence of chromosomal disorders in children with tetralogy of Fallot, such as Down syndrome and Di George's syndrome (a partial gene deletion that results in heart defects, low calcium levels, and immune deficiency.)
Symptoms
•Difficult feeding (poor feeding habits)
•Failure to gain weight
•Poor development
•Cyanosis which becomes more pronounced during periods of agitation
•Passing out
•Sudden death
•Clubbing of fingers (skin or bone enlargement around the finger nails)
•Squatting during episodes of cyanosis
•Stroke
Exams and Tests
A physical examination with a stethoscope almost always reveals a heart murmur.
Tests may include:
•EKG (electrocardiogram) may show the thickening of the right ventricle muscle
•CBC blood tests may show an increase in red blood cells
•Chest x-ray may show a "boot shaped" heart and dark lungs
•Cardiac catheterization helps show blood vessels in the lungs and heart
•Echocardiogram provides a definite diagnosis
•MRI of the heart (generally after surgery)
Treatment
Surgery to repair heart defects is always done when the infant is very young. Sometimes more than one surgery is needed. The first surgery may be done to help increase blood flow to the lungs. Surgery to correct the problem may be done at a later time. (Generally, a definitive corrective surgery is performed in the first few months of life.) Corrective surgery is done to widen part of the narrowed pulmonary tract and close the ventricular septal defect.
Tips for parents of children with tetralogy of Fallot:
•If a child does become blue, immediately place the child on his or her side and put the knees up to the chest. Calm the baby and seek medical attention immediately
•Feed the child slowly
•Give smaller, more frequent meals
•Decrease the child's anxiety by remaining calm
•Minimize crying by trying to anticipate the child's needs
•Recruit others to care for the child to prevent yourself from becoming exhausted
Outlook (Prognosis)
Most cases can be corrected with surgery. Babies who have surgery usually do well. Ninety percent survive to adulthood and live active, healthy, and productive lives. Without surgery, death usually occurs by the time the person reaches age 20.
Patients who have continued, severe leakiness of the pulmonary valve may need the valve replaced.
Regular follow up with a cardiologist to monitor for life-threatening arrhythmias (irregular heart rhythms) is recommended.
Possible Complications
•Delayed growth and development
•Seizures during periods of insufficient oxygen
•Arrhythmias
•Death
When to Contact a Medical Professional
Call your health care provider if new unexplained symptoms develop or if the patient is having an episode of cyanosis (blue skin).
Prevention
There is no known prevention.
Alternative Names
TET; TOF
References
Zipes DP, Libby P, Bonow RO, Braunwald E, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine, 8th ed. St. Louis, Mo; WB Saunders; 2007.

Tetralogy of Fallot